My Story
I remember the day exactly.
It was a cold Sunday morning in Portland, Oregon, and my two-month-old baby lay sleeping in her basinet. The dishes were done and my husband was on the couch dozing off as well. Something told me that I was ready to attempt my first postpartum run.
I expected it to be a little humbling; I mean, you can’t just lace up your Asics after several weeks of wearing house slippers and pick up where you left off. I was an experienced distance runner (half-marathons were my specialty), and this wasn’t my first hiatus; I’d taken time off for injuries and illness, and I had no reason to believe that this time would be any different.
I had a lot to learn.
I was only a few blocks away when something happened. And it happened all over my new running tights.
I had a cold, bowlegged walk home, followed by a thoroughly unsatisfying post-run shower. Then came the humiliation of telling my husband that I had just had my first encounter with stress incontinence.
Before it affected my life, I thought stress incontinence (inadvertently peeing when you put pressure on your pelvic floor) was an problem for the old and infirm. Actually, about 20% of the population—and about 50% of new mothers—struggle with this issue every day.
The limitations this put on my life were significant: running was out. Calisthenics? Out. Chasing after my nephews, running for a train, dancing at a nightclub?
Out, out, out.
There has to be a solution, I thought—and, with the same enthusiasm I once took the running trails, I jumped headlong into pelvic floor repair. I hired a physical therapist and took dozens, if not hundreds, of postpartum yoga classes.
And: I kegeled. On the bus, at the store, during sex. I kegeled and I kegeled and I kegeled.
The final straw came about six months into physical therapy treatment, when my PT pulled the thin fabric curtain between us and had me insert a biofeedback monitor to measure my vaginal contractions. After a moment she peeked over the curtain to ask: “Are you sure you’re squeezing?”
Since I had started seeing her, I had gotten weaker.
When I got back home I told my husband, through spasms of sobs, what had happened. How my body had betrayed me; how I was working harder but getting weaker. How my body—my life—would ever be the same again.
Fortunately, I had a secret weapon in the battle against stress incontinence: my husband is Kevin Moore, an experienced movement therapist and Pilates instructor. Starting that night, after dinner and when our daughter was finally asleep, we researched human anatomy and devised new exercises to target the intricate muscles that comprise the pelvic floor. Kevin started to merge his astonishing discoveries about side-dominance behavior—the foundations of which would later become the Reembody Method—with the latest in Pilates and physical therapy techniques.
Through my research I discovered a curious irony: my case was particularly severe because I had been so active before childbirth. I had essentially locked down my pelvic floor muscles to the point where they were firing together, as a unit, and not as a sequenced reaction to environmental forces. So, my kegels were strong—but when I was doing anything that involved coordinating my pelvic floor with its neighboring muscles, I lost control.
Within a matter of weeks, I was seeing improvement: not just in my pelvic-floor control, but in the confidence that this new routine instilled in me.
My Pelvic-Floor Solution
Here’s a short video on what I did to recover from stress incontinence (explained in the text below):
Conventional perspective of human locomotion goes like this: we use our brain to contract our muscles, which moves our bones. In fact, environmental forces like gravity, friction and air pressure are the primary sources of movement in our skeleton; the role of muscle is to siphon off some of this force as it passes through the bones to be stored and released for later use. (This is as true for your hands as it is for your lower extremities.) This means that conscious gripping actions, like kegels, are only a small part of the puzzle.
The pelvis is propelled through space through the combination of two actions: rotating and shifting. The muscles of the pelvic floor contract in time with these big, structural motions, siphoning off momentum to power the mechanisms that control the organs held within.
If your pelvic floor is malfunctioning, it’s probably out of sync with your pelvic rotation, pelvic shift, or both. By identifying which of these motions are limited, we can pinpoint the moment the pelvic floor loses connection with the surrounding structure and is forced to contract on its own: something it is not designed to do indefinitely.
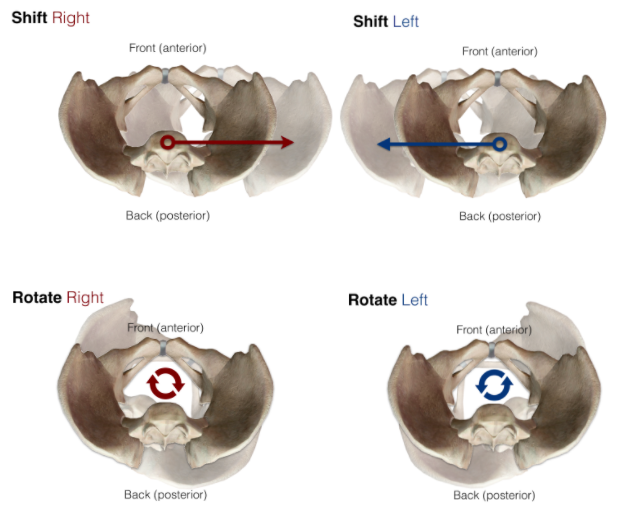
Shift right, shift left, rotate right, rotate left. That’s it. That’s all your pelvis does.
The vast majority of people follow the same pattern of vulnerability:
-
- Shifting toward the dominant side and rotating toward the non-dominant side—either together or as separate motions—generates pelvic floor tightness (over-facilitation).
- Shifting toward the non-dominant side and rotating toward the dominant side—either together or as separate motions—generates pelvic floor weakness (under-facilitation).
This is primarily because we do not use the motions of shifting toward the non-dominant side and rotating toward the dominant side frequently enough during our normal gait for the nervous system to have robust proprioception of this action.
For example: I am right side-dominant, so my weakest corner is shifting left/rotating right. I began to incorporate this action into kettlebell complexes, deadlifts and even sleeping (propping up my left hip on a pillow). I also eased off the kegels, allowing my pelvic floor to contract only as needed during routine activities.
The real magic happened when I applied these cues to my movement routine; integrating the “dominant hip back” cue was a game changer, particularly during runs. I built up my running routine slowly, alternating between walking and jogging until I felt comfortable.
Do I still struggle with stress incontinence? I’m thrilled to say that I haven’t had an incident in years—but I do make time to practice these exercises every day.
At best I’m cured; at worst, I’m in remission.
And I can live with that.
Your Custom Pelvic Floor Solution
-
- Standing comfortably, gently contract your pelvic floor.
- Next, move into one of the pelvic positions described above. Note whether your pelvic floor contraction was affected by your move. Did it weaken? Strengthen? Was it more comfortable? Less?
- Repeat with each of the actions above, allowing for ample recovery time between motions. Squeeze very gently; try to get a sense of which muscles you are using.
- Now, try combinations: gently contract the pelvic floor and then shift left and rotate right.
- Repeat with each possible combination.
By exploring all possible movements, you can begin to anticipate where the pelvic floor is at its weakest and at its most over-recruited.
Exploring those ranges is the most powerful intervention for repairing pelvic floor function.

Leave A Comment:
Your email address will not be published.